A version of this article appeared in FocusforHealth.org. Edited and republished with permission.
Edited by Louise Kuo Habakus
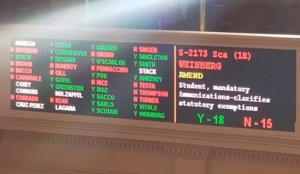
In the current debate over whether or not to legislate the removal of individual vaccine exemptions, fear of disease prevails. The quality of the vaccines themselves gets little attention. Scroll down or click to jump to references.
When vaccines are not effective
According to the CDC, mumps outbreaks are on the rise despite the fact that 94.6% of children in the U.S. have had two doses of MMR vaccine. To combat the situation, the CDC is considering adding a third dose of MMR to the recommended vaccine schedule.
In 2010, California experienced the largest pertussis epidemic since 1958. According to the CDC, the U.S. has experienced increased pertussis disease despite high levels of vaccine coverage resulting from the six doses (5 DTaP and 1 Tdap) that CDC recommends all children to receive. Researchers studying the pertussis outbreaks determined vaccine effectiveness dropped to less than 9% by four years, and that the quality of immunization waned so rapidly that little protection remained 2-3 years after vaccination.
Influenza vaccination has had no beneficial effect on flu mortality. The CDC indicates vaccine effectiveness has oscillated between 10-60% from 2005-2017, while systematic reviews show little to no benefit of inactivated influenza vaccines on flu morbidity.
The logic of forcing a failing vaccine?
It’s clear that some vaccines don’t work as well as advertised. And yet, instead of first making a vaccine with better effectiveness, the solution is to use the force of law to make everyone get more shots of the failing vaccine.
Even when significant vaccine failure rates for vaccines are acknowledged, the legislative solution remains fully supported. Concerns over the need for more effective vaccines are dismissed by apologists pointing out that the current vaccines are better than nothing. The assumption is implicit: low immunity is better than no immunity. So, until a better vaccine comes along, accept the current shot at whatever level of immunity it provides.
Worse than nothing, they’re spreading disease
But the notion that any amount of antibodies is preferable to no antibodies at all is dangerously wrong. The same exact antibodies that prevent disease at higher concentrations can enhance the disease at lower concentrations.
Instead of preventing infection, the antibodies permit a more invasive spread of the virus into different cell types, enhancing the disease and making it worse than if the child had never been vaccinated. This phenomenon is called antibody-dependent enhancement of disease, and it is a potential problem for vaccines that induce low levels of antibodies.
It’s not just a theoretical concern. It has happened. Vaccine-induced disease enhancement occurred previously with a measles vaccine that produced low levels of immunity.
From Iankov et al. 2006
An unexpectedly severe form of measles (atypical measles) was observed in immunized persons in the mid-1960s
Three doses of measles vaccine induced a short-lasting humoral immune response, followed several months or years later by susceptibility to atypical measles
Antibodies recognizing measles virus can increase the efficiency of virus entry into cells of the monocytic lineage
Antibody-mediated enhancement of infection may also contribute to cytokine alteration and modulation of the innate immune mechanisms during measles
The results point to an additional pathogenic mechanism that may be in play during measles virus infections and which may have particular relevance to the pathogenesis of the atypical measles that is seen after immunization
The effect of vaccine-induced disease enhancement has been seen in clinical trials for a since abandoned HIV vaccine.
From Huisman et al. 2009
Certain experimental vaccines have proved to be counterproductive: they rendered vaccinated subjects more susceptible to infection rather than protecting them
For candidate HIV vaccines a number of phase III trials have been conducted in seronegative volunteers at high risk for HIV infection
The outcome of these trials was far from encouraging, with very limited induction of HIV neutralizing antibodies, and no evidence for protection
In one clinical trial, a significant trend towards increased HIV-1 infection was observed
Antibody-dependent enhancement of infection remains a significant concern in the development of safe and effective vaccines
There may well be a delicate balance between the induction of protective immunity on the one hand and the induction of enhanced susceptibility on the other
The HPV vaccine exhibited the capacity to enhance HPV infections during clinical trials. Women who tested positive for vaccine HPV serotypes by PCR analysis, and were then administered the vaccine, were more likely to develop high-grade cervical lesions than the non-vaccinated control group. These observations have persisted beyond clinical trials, and antibody-dependent enhancement has been raised as a possible explanation.
From Manos 2009
Vaccination of women with previous HPV 16 or 18 infection might actually increase their risk of high-grade cervical disease
This observation is strikingly consistent with reports on the quadrivalent HPV vaccine
Although each trial’s finding was attributed to imbalances in the baseline characteristics of the vaccine and placebo groups, the biological phenomenon of antibody-dependent enhancement of disease should be considered
Perhaps HPV testing should precede vaccination and be contraindicated for women and girls previously infected
Flu vaccines increase risk of getting flu
It’s been known for decades that non-neutralizing influenza antibodies can augment the uptake of influenza A virus strains, but it wasn’t until recently that the phenomenon of disease enhancement for influenza vaccination was observationally proven.
In 2009, seasonal influenza vaccination increased the risk of pandemic influenza illness in those who received the vaccine. This result was confirmed in four observational studies.
Ineffective vaccines are a bad thing
Antibody-dependent enhancement of disease has been proposed as the potentiating mechanism.
Vaccines sometimes do nothing ─ they cause no harm as they fail to protect the vaccine recipient from disease.
Vaccines sometimes do worse than nothing ─ they cause more cases, and more severe cases of disease in those who opt to be vaccinated. Low levels of antibodies cannot be viewed as less of a good thing. Ineffective vaccines are a bad thing. They stimulate low level immune responses that sometimes potentiate the exact diseases they were intended to prevent.
Abandon coercive laws and ineffective vaccines
Legislation that would force the use of an ineffective vaccine must be abandoned. But that’s not enough. The ineffective product itself must be abandoned. According to the FDA, vaccine policy that mandates usage of an ineffective vaccine leads to disease outbreaks in older age groups that are more likely to suffer complications from disease.
Vaccine policy aimed at preventing outbreaks and eradicating disease can only succeed when there is high vaccine uptake of an effective vaccine. If one is missing, there is no point in having the other.
The continued use of some of the current, poorly-performing vaccines, moots any perceived necessity to legislate forced uptake, because no amount of vaccine uptake will prevent disease outbreaks. Even with 100% compliance, outbreaks would still occur because the vaccines are not effective enough to provide population level immunity sufficient to prevent epidemics.
Furthermore, outbreaks will continue to occur in older age groups where complications from disease are more common, and mothers will have little to no immunity to provide to their newborns during those early critical months of life.
All individuals should have the legal right to exempt themselves and their children from using the current products. Let’s repeat what Huisman et al observed. Antibody-dependent enhancement of infection remains a significant concern in the development of safe and effective vaccines. It is precisely because of these and other concerns about safety and effectiveness that vaccines should not be mandated.
References
https://www.cdc.gov/mumps/outbreaks.html (PDF)
CDC. October 7, 2016. Vaccination coverage among children in kindergarten ─ United States, 2015-2016 school year. Morbidity and Mortality Weekly Report. 65(39):1057 (PDF)
CDC. July 29, 2016. Mumps outbreak at a University and recommendation for a third dose of measles-mumps-rubella vaccine ─ Illinois. Morbidity and Mortality Weekly Report. 65(29):731 (PDF)
CDC. July 9, 2010. Notes from the Field. Pertussis─California, January-June 2010, Morbidity and Mortality Weekly. 59(26):817 (PDF)
Klein et al. 2016. Waning Tdap effectiveness in adolescents. Pediatrics. 137(3):1 (PDF)
Simonsen et al. 2005. Impact of influenza vaccination on seasonal mortality in the US elderly population. Archives of Internal Medicine (165):265 (PDF)
https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm (PDF)
Jefferson. 2006. Influenza vaccination: policy versus evidence. British Medical Journal. (333):912/
Burton et al. 2000. Antibody and virus: binding and neutralization. Virology (270):1
Iankov et al. 2006. Immunoglobulin T antibody-mediated enhancement of measles virus infection can bypass the protective antiviral immune response. Journal of Virology. 80(17):8530 (PDF)
Huisman et al. 2009. Vaccine-induced enhancement of viral infections. Vaccine. (27):505
HPV vaccine (Gardasil) clinical trial data
Manos 2009. Lancet. (374):1328 (PDF)
Tamura et al. 1994. Subtype cross-reactive, infection-enhancing antibody responses to influenza A viruses. Journal of Virology. 68(6):3499 (PDF)
Janjua et al. 2010. Seasonal influenza vaccine and increased risk of pandemic A/H1N1-related illness: first detection of the association in British Columbia, Canada. Clinical Infectious Diseases. 51(9):1017 (PDF)
Tsuchihashi et al. 2012. Association between seasonal influenza vaccination in 2008-2009 and pandemic influenza A (H1N1) 2009 infection among school students from Kobe, Japan, April-June 2009. Clinical Infectious Diseases. 54(3):381 (PDF)
Skowronski et al. 2010. Association between the 2008-2009 seasonal influenza vaccine and pandemic H1N1 illness during spring-summer 2009: four observational studies from Canada. PLOS Medicine. 7(4):1 (PDF)
Dutry et al. 2011. Antibody-dependent enhancement (ADE) of infection and its possible role in the pathogenesis of influenza. BMC Proceedings. 5(Suppl 1):62 (PDF)









Keep in mind that the mathematical formula they use to measure vaccine effectiveness for flu shots considers causing more respiratory illnesses to be equivalent to preventing flu so if the effect of the flu vaccine is to double your chances of getting flu and quadruple your chances of getting a respiratory illness they would compute that it has 50% effectiveness.